Our team of highly skilled oncologists, medical physicists and radiographers are committed to delivering the very best of care to our patients, using the latest radiotherapy machines and techniques.
The decision whether to use radiotherapy and which type of radiotherapy to use is made on a patient-by-patient basis.
Different tumour types respond to radiotherapy in different ways so all patients require an individualised treatment plan.
The Kent Oncology Centre offers radiotherapy treatments at two different sites – Maidstone Hospital and Kent and Canterbury Hospital.
Types of radiotherapy
The two main types of radiotherapy are:
External radiotherapy – where the radiation comes from a machine outside the body.
Internal radiotherapy – where the radiation comes from implants or liquids placed inside the body.
External radiotherapy
External radiotherapy is the most common type of radiotherapy used. It is usually given as a course of several treatments over days or weeks.
External radiotherapy is usually given during outpatient visits to a hospital cancer centre. A machine directs the high-energy radiation, usually X-rays, at the cancer site and a small area of normal tissue surrounding it. You will be positioned carefully on a treatment couch and then the machine will be directed exactly at the area to be treated, often from different angles. Treatment takes several minutes and is painless.
External radiotherapy doesn’t make you radioactive and you can safely mix with other people, including children, at any time during your treatment.
Internal radiotherapy
Internal radiotherapy can be given in several ways.
Brachytherapy is treatment in which solid radioactive sources are placed inside a body cavity or needles are placed in the tumour. This is usually given on an outpatient basis but may involve staying in hospital for a few days until the radioactive source has been removed.
Another type of internal radiotherapy involves using a liquid source of radiation and is called radionuclide (radioisotope or unsealed source) therapy. It can either be taken by mouth or given as an injection into a vein. For this type of treatment, you will need to stay in hospital for a few days until most of the radioactivity has disappeared from your body.
If you are going to have internal radiotherapy, your doctor will discuss this with you and give you further information.
Occasionally, with radioactive treatment or with treatment with radioactive ‘seeds’, you will be emitting a certain amount of radioactivity for a few days. This is why there may be temporary restrictions on your movements and visitors. This will be carefully explained to you.
Who will be treating me?
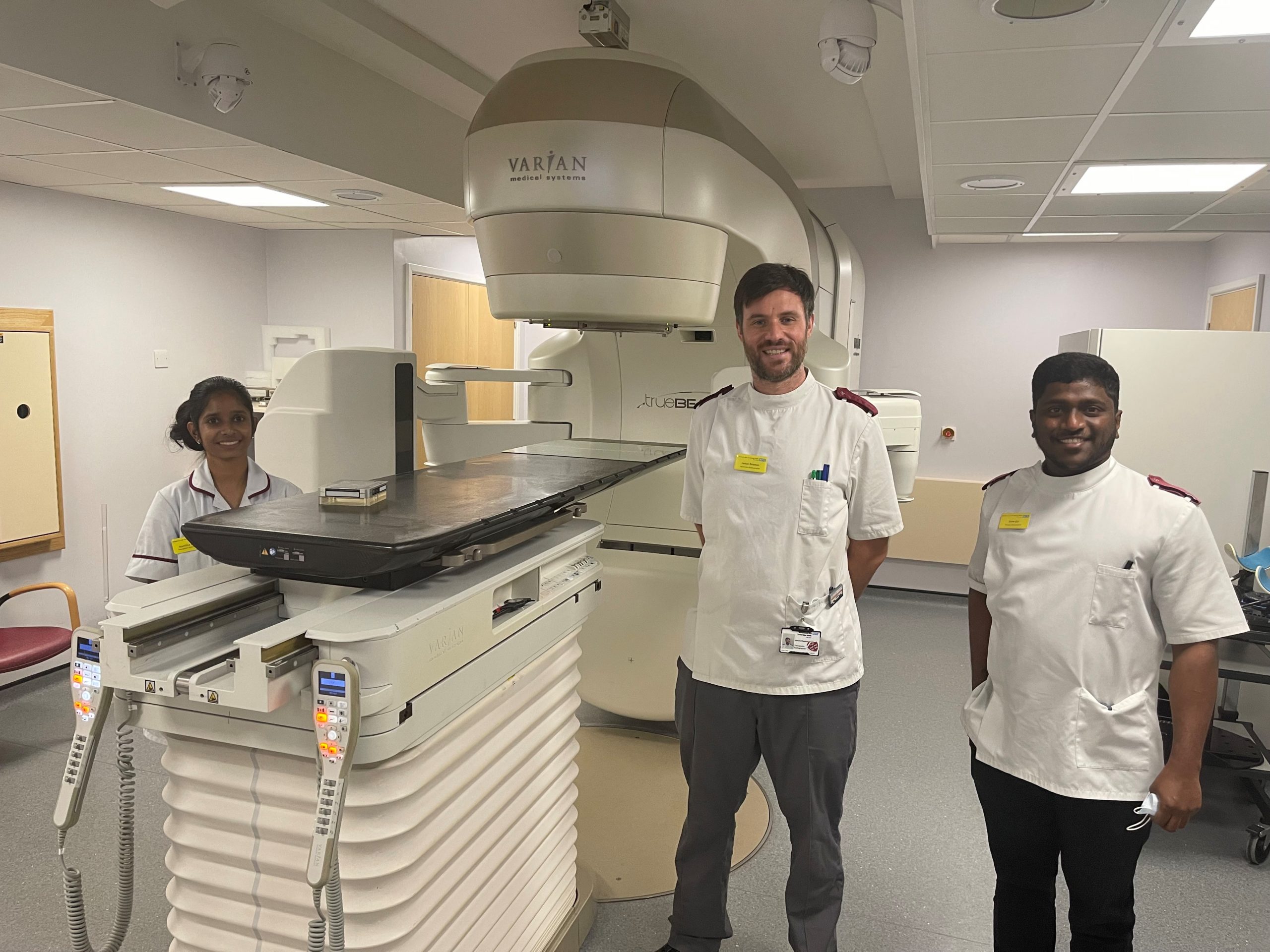
Therapy radiographers are the main people you will come into contact with when you have radiotherapy treatment. They work closely with the clinical oncologist and help plan and are responsible for giving you your treatment. They will be able to answer many of your questions. Radiographers are also able to advise on possible side effects and what you should or shouldn’t do during treatment.
Most cancer centres are also teaching hospitals so your team may include a student radiographer, student nurse or a medical student. Please tell us if you don’t want a student present during your clinic or treatment appointment.
During your treatment you may be seen in a review clinic. The exact number of times you are seen depends on the length and type of treatment you are having, as well as how you are feeling. In these clinics you will see a specialist nurse or a doctor. You may also see a dietitian if needed.
You may also meet nurses in the radiotherapy department; they can advise you on care during your treatment.
Receiving radiotherapy
How is the radiotherapy machine chosen?
There are several different machines used for giving radiotherapy and they each work in slightly different ways. The machine used will depend on many things, such as which part of your body is to be treated and why treatment is being given.
How many treatments will I have?
You may have a single treatment or a course of treatments, called fractions, over several weeks. This depends on why radiotherapy is recommended for you. Lower doses are given for palliative treatment than for curative treatment and usually over a shorter period of time.
When do I attend for treatment?
Radiotherapy is normally given, Monday to Friday as an outpatient. The number of treatments you will need depends on many facts about you and your particular type of cancer. This can vary from a single treatment to a number of weeks of treatment. A course of radiotherapy may last for six or seven weeks. Everyone is different, and your doctor will decide how many treatments are best for you.
Most people receive radiotherapy as outpatients, travelling to the department each day. You might like to ask a friend or relative to come with you.
The staff will explain where you need to go and will try to arrange an appointment time that suits you. You will usually be able to book all your appointments at the same time to allow you to plan ahead. If you are staying in hospital, the radiographers will arrange your treatment times with the ward staff.
What happens when I come for treatment?
Each time you visit for treatment a radiographer will ask you three questions to make sure you are the person they are expecting to treat. These are: your name, address and date of birth (even though they may know you).
You may be asked to change into a gown before treatment, and then the radiographers will position you on the couch. Using the tattoos or marks which were put on your skin during treatment planning, they will line up the radiotherapy machine. It won’t usually touch you.
The preparation may take some time, often longer than the treatment itself. It will probably take longer on the first day. When the radiographers are satisfied that you and the treatment machine are both in the correct position, they will leave the room and switch on the radiation beam. You won’t feel anything during the treatment.
The radiographers will watch you using closed-circuit television or through a window. You can speak to them and they can speak to you via an intercom. You should keep very still during the few minutes it takes to give your treatment but you can breathe and swallow normally. The machine may move around you during treatment, or the radiographers may come in to change your position or that of the machine. They will explain each step to you.
What are the side-effects of radiotherapy?
You may need to reduce the hours that you work or cut back on social or sports activities. Make sure you get enough rest and accept offers of help with everyday tasks or jobs. If you are worried about anything, or would just like to talk, your doctor, radiographer or nurse will be happy to listen or advise.
The radiographer will check your progress regularly during your treatment and you will see the doctor or nurse from time to time in a clinic. If you have questions at any time, do ask.
Radiotherapy side effects
The side effects you may experience will depend on the part of the body that is being treated and how much treatment you have. Side effects only affect the part of the body that is treated. Everyone reacts to radiotherapy differently and many people have hardly any side effects. The radiographers will give you lots of support and advice to care for and manage the side effects.
You will also be given written information about the side effects relevant to your treatment. Most side effects are temporary and they are rarely severe. They may start at varying times during treatment and disappear in the weeks after the end of it. Some side effects may not start until treatment is finished.
Tiredness
Radiotherapy can make you feel more tired than usual. You should listen to your body and rest if you need to but continue your normal activities if you feel able. Some people are able to continue working but others find they are too tired. Tell your radiographer or doctor if tiredness is a problem. They may be able to offer advice on ways to save your energy and cope with everyday activities.
Nausea and vomiting
A few people feel sick during radiotherapy – it depends on which part of the body is being treated. Some people feel sick at the beginning of a course of treatment but find that nausea often disappears within a day or two. Others start to feel sick later on.
Hair loss
Radiotherapy can cause hair loss in the area being treated. Most hair loss is temporary and will start to grow back within two to three months of finishing treatment.
Sore skin
There is currently no general agreement based on research regarding caring for skin during radiotherapy. Advice on skin care varies from one hospital to another. The staff at your radiotherapy department will give you advice about how to care for your skin in the treatment area at the beginning of your course of radiotherapy.
During treatment the skin may become red and sore and it’s important not to irritate it. Avoid shaving within the treatment area. You may wash the area gently using a mild unperfumed soap, such as baby soap, and pat it dry. Don’t use any deodorants, perfumes or lotions on your skin other than those recommended by the team caring for you. You should protect your skin from extremes of temperature and continue using sunscreen (factor 15 or above) after your treatment has finished.
Clothing
You may find it more comfortable to wear loose, casual clothing made from natural fibres. If you have ink marks on your skin from your treatment, you may find they smudge onto your clothes. Stains can be removed from your clothes using a biological washing powder. However, you may wish to wear older or less special clothes during your treatment.
Joint or muscle stiffness
Occasionally people who have radiotherapy to areas over joints or muscles may experience some stiffness. This can occur at any time up to two years after treatment has finished. Regular exercise to these joints and muscles can prevent stiffness. Your doctor may refer you to a physiotherapist. If not, please ask for advice.
Patient information leaflets
The Kent Oncology Centre produces a range of informative leaflets for patients. Read or download a copy here.
Radiotherapy
- Electron Beam Radiotherapy – Treatment and Planning
- External Beam Radiotherapy
- External Beam Radiotherapy for Prostate Cancer: Preparing for your CT scan and treatment
- Finishing Radiotherapy
- Advice about using dilators after Radiotherapy
- Radiotherapy side effects and management – Anal Cancer
- Radiotherapy side effects and management – Bladder Cancer
- Radiotherapy side effects and management – Bone Cancer
- Radiotherapy side effects and management – Bowel Cancer
- Radiotherapy side effects and management – Brain Cancer
- Radiotherapy side effects and management – Breast Cancer
- Radiotherapy side effects and management – Gynaecological Cancer
- Radiotherapy side effects and management – Head and Neck Cancer
- Radiotherapy side effects and management – Lung Cancer
- Radiotherapy side effects and management – Oesophageal Cancer
- Radiotherapy side effects and management – Pituitary Adenoma and Craniopharyngioma
- Radiotherapy side effects and management – Prostate Cancer
- Radiotherapy side effects and management – Thyroid Cancer
- Side effects and management for Radiotherapy to Chest, Neck and / or Axilla
- Side effects and management for Radiotherapy to the Abdomen
- Side effects and management of a short course of Radiotherapy to the pelvis
- Side effects and management of Radiotherapy to the groin
Brachytherapy